What is Hypnosis?
The question, “what is hypnosis?” is easier to ask than to answer. Science has been fascinated by the study of the complex phenomenon of hypnosis, and if you ask different people, you’ll be offered different answers. So far, there has been no one widely accepted definition of hypnosis. It might be better to consider hypnosis in terms of explanatory “models” rather than formal definitions.
The term ‘hypnosis’ was coined by James Braid, a Scottish surgeon in the 19th century because he thought it represented a state of sleep. Hypnosis became an accepted form of treatment popularised by Freud, Breuer, and Charcot in the nineteenth and early twentieth century. Before the advent of anaesthesia, Esdaile used hypnosis surgically and reduced operative mortality by 90% ((Wobst 2007). But when Freud later rejected it in favour of psycho analysis it fell into disuse until after the Second World War. Now with the advent of advanced imaging techniques, hypnosis has been used in neuro -physiological research and has found its place in areas of clinical treatment and recommended within NICE guidelines.
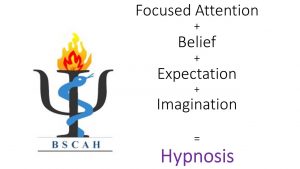
When the word hypnosis is used generally, it is often associated with stage shows, implying a sort of magic, a loss of control, disinhibited behaviour, and entertainment. Some people regard this as ‘scary fun,’ but for others the idea of giving up personal control to someone else is justifiably scary. When health professionals use hypnosis, they educate the patient that hypnosis is a very natural state involving focused attention, and in fact, it will give them more choice and control over their experiences and symptoms.
Hypnosis can be seen as ‘a waking state of awareness, (or consciousness), in which a person’s attention is detached from his or her immediate environment and is absorbed by inner experiences such as feelings, cognition and imagery’. Heap M. Hypnotherapy – a handbook. 2nd ed. Milton Keynes, UK: Open University Press, 2012.
Hypnosis, therefore, when used skilfully by a clinician, is a “vehicle” for therapeutic content.
Hypnosis is “A state of consciousness involving focused attention and reduced peripheral awareness characterized by an enhanced capacity for response to suggestion.” American Psychological Association 2014.
A key component of hypnosis is focused attention. How that is achieved in order to reach a state that is different from both wakefulness and sleep is fascinating. This narrowed focusing of attention is neurobiologically rooted- it is an ability of the human brain. Described in this way, hypnosis occurs naturally when we become deeply absorbed or entranced during everyday life. There are many experiences which involve hypnotic responding with this focused attention. For example, playing video games; watching TV; praying; reading; running; getting lost in thought- all can involve a narrow focus of attention, such that we begin to lose awareness of things going on around us.
The importance of recognising and studying this state of mind comes because it also occurs at times of emotional distress e.g., following a trauma; being in pain et cetera. A person in this state becomes powerfully receptive at an unconscious level to suggestions. As clinicians it is useful to recognise and be sensitive to this vulnerability, and then be able to turn the vulnerable state into a basis for effective treatment. This can be used to reduce emotional pain and distress, and physical pain. Hence its importance in all clinical work, and the inherent dangers of hypnosis used by non-professionals for clinical applications.
What is an Induction?
In clinical work, this focused state is achieved by using the “hypnotic induction”. Induction is the process by which a patient enters hypnosis (Simons, Potter, & Temple 2007). This does not involve a pocket watch, but instead, the use of carefully chosen words in the context of a helping therapeutic relationship, designed to unlock the power of a relaxed and focused state. The health professional or researcher suggests that the person experiences changes in sensations, perceptions, thoughts or behaviour within a hypnotic context. There are many different methods of performing an induction, and hypnosis training courses spend lots of time looking at a range. A clinician who uses hypnosis should be familiar with a number of different inductions and match them to the needs of the individual patient. Although there are many different hypnotic inductions, most include suggestions for relaxation, calmness and well-being. Guidance to imagine or think about pleasant experiences are also commonly included in hypnotic inductions. If a patient is highly anxious or in shock they may already be in a hypnotic state so little, or no induction is required. BSCAH teaches healthcare professionals to recognise and utilise this as well as teaching the formal inductions to engage the patient’s imagination.
How would I feel in hypnosis?
People respond to hypnosis in different ways. Some describe their experience as an altered state of consciousness or similar to a meditative state. Others describe hypnosis as a normal state of focused attention, in which they feel very calm and relaxed. Regardless of how and to what degree they respond, most people describe the experience as very pleasant. You can still speak in hypnosis although it might feel an effort to do so and at all times you can decide not to follow the suggestions being given and re-alert yourself. A hypnotic induction is not like a light switch. At different times you may be more focused inwards or become more aware of your surroundings.
Can anyone be hypnotised?
Some people are very responsive to hypnotic suggestions and others are less responsive. A person´s ability to experience hypnotic suggestions can be inhibited by fears and concerns arising from some common misconceptions. Contrary to some depictions of hypnosis in books, movies or on television, people who have been hypnotised do not lose control over their behaviour. They typically remain aware of who they are and where they are, and unless amnesia has been specifically suggested, they usually remember what transpired during hypnosis. Hypnosis makes it easier for people to experience suggestions, but it does not force them to have these experiences. Hypnosis should not be used in certain conditions such as acute psychoses.
What can hypnosis be used for?
Hypnosis isn’t a treatment in its own right, but when used by a qualified doctor, dentist, or other clinician, hypnosis can be helpful in treating: pain, anxiety conditions (including phobia, panic, PTSD), depression, irritable bowel syndrome, and many more. However, it may not be useful for all clinical problems or for all patients or clients. The decision to use hypnosis as an adjunct to treatment should only be made in consultation with a qualified healthcare provider who has been trained in the use and limitations of clinical hypnosis.
Hypnosis is not a type of therapy, like psychoanalysis or behaviour therapy. Instead, it is a procedure that can be used to facilitate therapy. Because it is not a treatment in and of itself, training in hypnosis is not sufficient for the conduct of therapy. Clinical hypnosis should be used only by properly trained and credentialed healthcare professionals (e.g. licensed clinical psychologists), who have also been trained in the clinical use of hypnosis and are working within the areas of their professional expertise.
In addition to its use in clinical settings, hypnosis is used in research, with the goal of learning more about the nature of hypnosis itself, as well as its impact on sensation, perception, learning, memory, and physiology. Researchers also study the value of hypnosis in the treatment of physical and psychological problems.
Is hypnosis dangerous?
In the UK, hypnosis is unregulated so there is nothing preventing people from simply practicing hypnosis even when they lack the necessary skillset.
Hypnosis is safe; it is the suggestions delivered whilst in hypnosis that could lead to negative reactions. Untrained professionals might use suggestions inappropriately or not be able to tell if another treatment is more suitable for you. If a therapist uses suggestions incorrectly, they can create false memories that may not be accurate without meaning to. Therefore, hypnosis should always be performed by a qualified healthcare professional.
If your hypnotherapist can’t treat your condition without hypnosis, they shouldn’t be treating you with hypnosis.
Hypnosis can be dangerous for people with serious mental disorders such as: Schizophrenia, sufferers of hallucinations or delusions.
I am a healthcare professional – should I learn to use hypnosis?
The answer to this question is YES. The education that BSCAH provides will help you to build on your existing clinical communication skills. You will learn to use language more skilfully and effectively – and avoid giving inadvertent negative messages (nocebo language). You will be able to teach your patients how to use coping skills and strategies to manage their conditions in a way that is empowering. You will learn how to use self-hypnosis to become more relaxed and resilient – and teach these important skills to your patients.
Clinical hypnosis has been used to treat pain (acute and chronic), nausea, anxiety, phobias, functional disorders and many other clinical conditions. It can be helpful in speeding recovery post-surgically. It is useful in anaesthesia, and in managing medical procedures more confidently and comfortably. Children respond very well to hypnosis in general.
BSCAH teaches ‘Adjunctive clinical/medical/dental hypnosis’ how is this different from hypnotherapy?
Adjunctive Clinical Hypnosis is used by healthcare
professionals such as doctors, nurses, dentists, and psychologists to
complement medical, dental and psychological treatments, helping with pain
management, functional disorders, nausea, anxiety reduction, behavioural
changes and more within a clinical setting. In contrast, hypnotherapy is
typically a standalone ‘therapy’, often practiced in private settings, to
address issues like phobias, smoking cessation, and personal development.
Adjunctive Clinical Hypnosis is always applied within a regulated healthcare
context by trained healthcare professionals who integrate hypnosis into
their existing medical, dental or psychological expertise. Adjunctive clinical
hypnosis is evidence-based and specifically designed to enhance conventional
treatments in healthcare.
How do I know that my therapist is suitably qualified?
First of all, consider whether you should see your GP or other healthcare professional to have your health issues diagnosed. Check your potential therapist’s qualifications and experience. Ask them plenty of questions before agreeing to be treated by them. Because hypnosis is not a “stand alone” treatment, enquire as to what type of approach or suggestions might be offered within the hypnotic framework. Make sure that you feel comfortable with their answers, and they take your concerns seriously. Make sure they have appropriate Indemnity insurance in place.
